Better understand diabetes to better prevent it
Published on 24/11/2025

Having type 2 diabetes means having too much sugar (glucose) in the blood continuously. This condition is known as chronic hyperglycaemia.
Diabetes appears when the body’s cells can no longer absorb sugar properly because they become less sensitive or resistant to insulin.¹˒²
What is insulin?¹
Insulin is a hormone produced by the pancreas. It allows the body to turn glucose into energy. Type 2 diabetes is the most common form.
🔵 It usually appears after the age of 40, but it can also occur earlier.
🔵 It develops slowly and often goes unnoticed for a long time.

How to react?
If you believe you might be at risk of developing type 2 diabetes, or if you have any questions, you can consult your general practitioner.
The first step is to talk to your general practitioner about your potential risk of type 2 diabetes. Your doctor can assess your overall health and discuss the next steps with you. This may include a few simple tests, such as checking your blood values. For accurate results, you need to come in sober, which means not eating or drinking anything in the morning before your appointment.
Key figures³
One in ten people lives with some form of diabetes. This represents more than one million Belgians.
90% of adults living with diabetes are affected by type 2 diabetes (T2D).
At the time of diagnosis, 30% of people with type 2 diabetes already show complications.

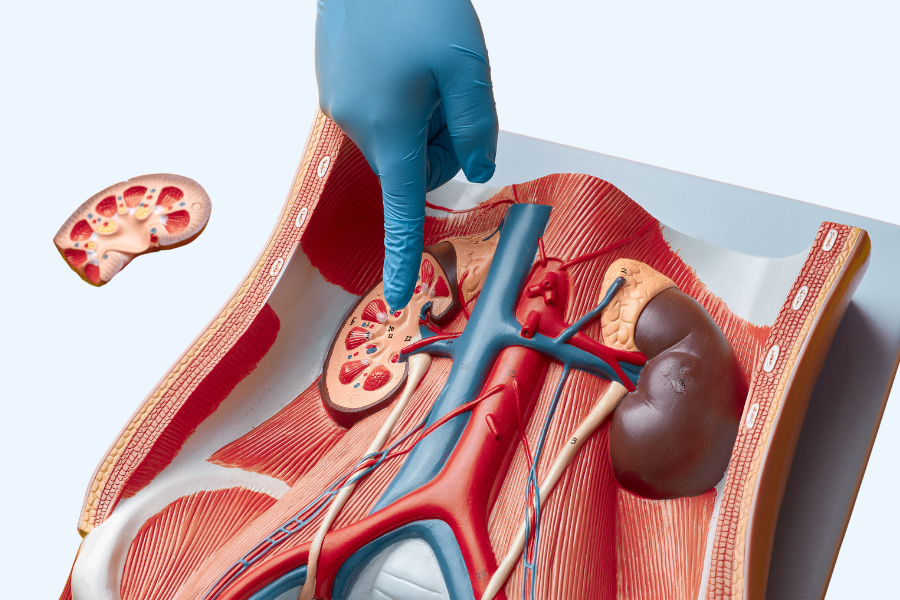
What is type 2 diabetes?¹˒²
The main hormone involved in type 2 diabetes is insulin. It is produced by the pancreas and regulates blood sugar levels. Without insulin, glucose remains in the bloodstream and blood sugar rises. Two main mechanisms lead to type 2 diabetes:
👉 A decrease in the cells’ sensitivity to insulin: Over time, or due to an excess of body fat (for example with overweight or obesity), the body’s cells become less responsive to insulin. Glucose enters the cells less easily and begins to build up in the blood. This is how hyperglycaemia gradually develops.
👉 Reactive hyperinsulinaemia or insulin deficiency: The pancreas produces more insulin for several years to compensate, but this requires constant effort. Over time, it becomes exhausted and can no longer produce enough insulin. Blood sugar then remains high on a long-term basis. This is type 2 diabetes.
Several genetic and environmental factors can increase the risk of diabetes.
✅ The main risk factors are:
- Age
- Family history
- High blood sugar
- High blood pressure
- Excess body weight
- An unhealthy lifestyle
- Smoking
- Metabolic syndrome (a combination of abdominal obesity, high blood pressure and high cholesterol)
Taking care of your health and adopting a balanced lifestyle helps stabilise blood sugar levels and reduces the risk of diabetes. If you have several risk factors, even under the age of 40, talk to your doctor. A diabetes risk test may be recommended.
Why is regular monitoring essential?¹
Type 2 diabetes is often silent and painless. More noticeable symptoms may appear later, such as intense thirst, dry mouth, frequent urination, unexplained tiredness or blurred vision. The diagnosis is often made by chance, during a medical check-up or following a complication.
It is possible to live with diabetes without being aware of it. During this time, complications may already be developing. Regular check-ups with a healthcare professional are therefore important to detect diabetes early and prevent long-term complications. If blood sugar remains too high for too long, this can lead to:
- Eye problems
- Cardiovascular diseases
- Foot complications
- Kidney issues
- Liver disorders
If you think you might have one of these complications, talk to your doctor about regular screenings or a preventive health assessment.
Preventing diabetes
Although heredity and age play a role, type 2 diabetes can be prevented in many cases. The key is adopting a healthy lifestyle.
Quitting smoking, being physically active and following a balanced diet all help reduce the risk of developing type 2 diabetes.
You can consult a doctor, dietitian, nutritionist or another healthcare professional for support.
Article written by Eli Lilly Belgium, in partnership with Doctena.
Sources:
1. Diabetes.be
2. Davies MJ, et al. Diabetes Care. 2022;45(11):2753-2786
3. Gezondbelgie.be/nl/gezondheidstoestand/niet-overdraagbare-aandoeningen/diabetes
Disclaimers:
CMAT-04480 – Nov 2025 E.R.: ELB, Rue du marquis 1/4B,
1000 Bruxelles© 2025



